Mallory-Weiss Tear Treatment
Most stop bleeding on their own, but 10-20% cause persistent upper‑GI hemorrhage that can strain operating room (OR) schedules, transfusion budgets, and bed capacity. Hospital teams need hemostasis tools that work quickly and fit easily into established endoscopy workflows.

Traditional Mallory-Weiss tear treatment options — clips, epinephrine injections, or multipolar cautery — remain common in the field. However, recurring bleeds, especially in frail or anticoagulated patients, can double procedure times and lengths of stay.
Recent advances in endoscopic laser coagulation promise a tighter seal with less collateral damage. The sections below explain why that matters to gastroenterologists, operations managers, and medical‑device resellers alike.
Understanding Mallory-Weiss Tears
Mallory-Weiss tear patients often present with hematemesis (vomiting blood), mild to moderate epigastric pain, or melena (dark, tarry stools). Typical causes include:
- Bouts of severe vomiting from alcohol intoxication or gastrointestinal infections
- Chronic cough or convulsions
- Strenuous physical activity that raises intra-abdominal pressure
Because these tears lie at the junction of the esophagus and stomach, diagnosing and treating them efficiently is essential to preventing rebleeding episodes.
Traditional Approaches to Mallory-Weiss Tear Treatment
When a patient arrives with a suspected Mallory-Weiss tear, clinicians typically begin by stabilizing vital signs and addressing any significant bleeding. This includes:
- Intravenous (IV) fluids if hypovolemia is suspected
- Blood transfusion in severe anemia or rapid blood loss
- Proton pump inhibitors (PPIs) to lower gastric acidity and create a stable environment for clot formation
Endoscopy is then performed to locate and assess the tear.
If the tear is actively bleeding or at high risk of rebleeding, endoscopic therapies such as injection (e.g., epinephrine), clipping, or thermal coagulation may be used.
These methods work well in many cases. However, rebleeding can still occur if the underlying vessel is not sealed correctly or if the patient’s condition predisposes them to ongoing mucosal trauma. Each failure means another procedure, additional anesthesia, and higher cost per case.
Why Consider Endoscopic Lasers?
A contact‑free laser fiber delivers photocoagulation directly to the bleeding point. Energy absorption by hemoglobin and water seals the vessel while limiting thermal spread to 200–300 µm.
For clinical teams, that translates to:
- Rapid hemostasis: Coagulation usually occurs within a few 0.5‑second pulses, shaving minutes off average case time.
- Lower re‑intervention rate: Studies report less than 6% rebleed when laser is used as primary therapy.
- Preserved mucosa: Minimal charring reduces ulcer base size and postoperative pain, allowing earlier diet advancement.
From an operational standpoint, fewer repeat scopes and shorter room occupancy improve throughput. One tertiary center calculated an extra 40 endoscopy slots per year after adopting lasers for upper‑GI bleed treatment.
How Laser Therapy Fits into the Procedure
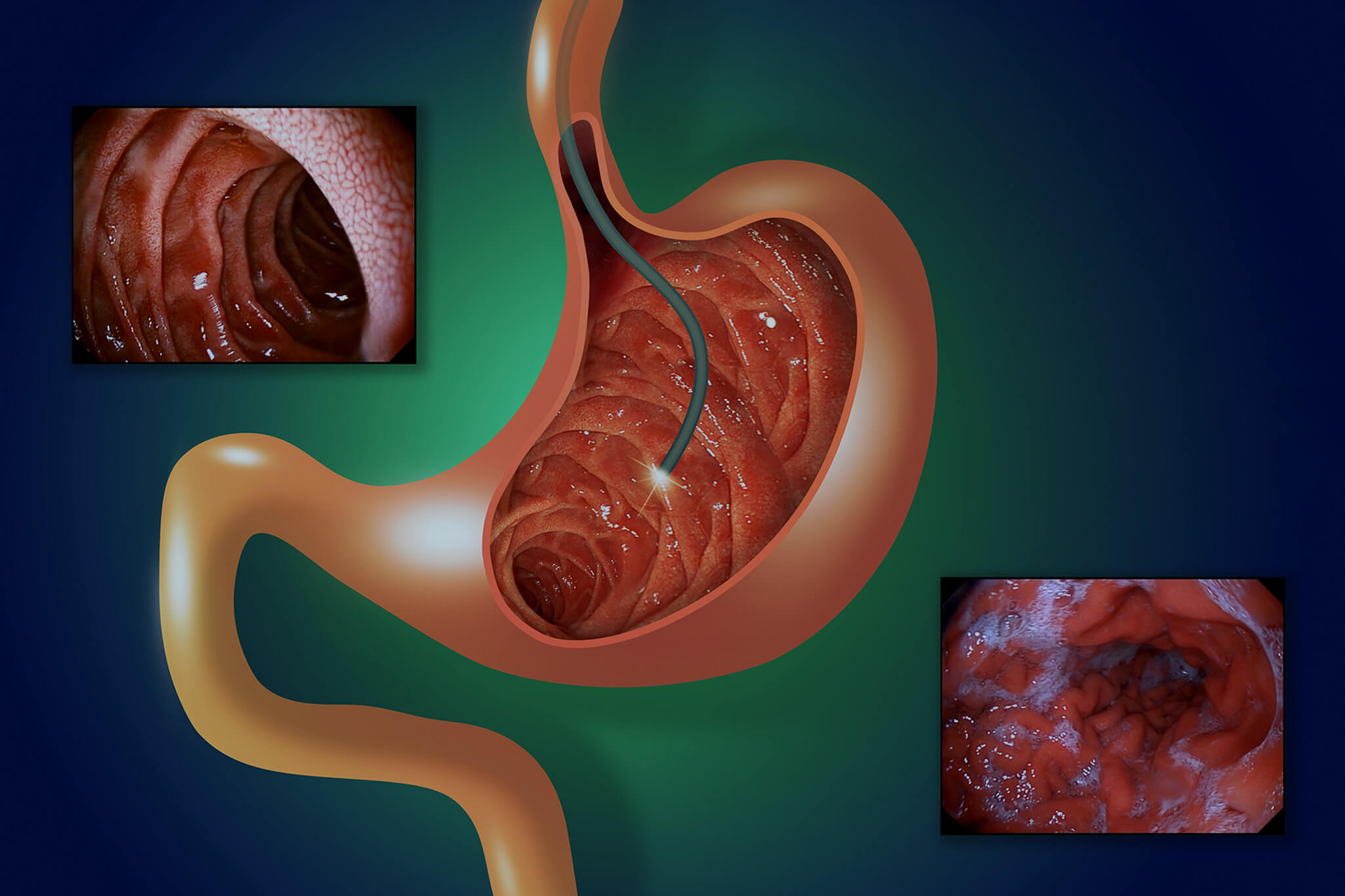
In laser-assisted Mallory-Weiss tear treatment, the physician uses an endoscope to visualize the bleeding site.
A specialized laser fiber is then guided through the working channel of the scope. The physician targets the tear or the exposed vessel and activates the laser in short, controlled pulses.
This approach has several benefits:
- Laser energy effectively cauterizes the bleeding area, creating a stable clot.
- It reduces thermal spread to adjacent tissue, which lowers the risk of deep necrosis.
- Patients often experience faster healing and less postoperative discomfort compared to some alternative techniques.

Benefits of Laser-Assisted Mallory-Weiss Tear Treatment
One of the greatest strengths of using lasers in GI endoscopy is the ability to achieve immediate hemostasis with reduced thermal spread. This results in less postoperative pain and fewer complications.
The short pulses of light energy seal the bleeding vessel quickly, and the procedure can be completed in a brief timeframe.
Endoscopic laser therapy also offers a high success rate for bleeding control. By applying short bursts of laser energy directly onto the tear, surgeons often see an immediate drop in active bleeding.
This helps limit the length of hospital stays and lowers the need for repeat endoscopies. Overall, patients may enjoy a smoother recovery and better comfort.
Potential Risks and Limitations
Though typically safe, laser treatment carries some risks. Thermal injury to deeper tissue layers is possible if power settings are too high or if the laser remains in contact with the mucosa for an extended period.
Additionally, equipment costs can be a barrier for smaller hospitals unless they form partnerships or shared ownership models to afford advanced laser platforms.
Patient selection remains essential. Individuals with coagulopathies or severe comorbidities may require more thorough supportive care.
In rare cases, a tear that extends deeply into submucosal layers or an actively pulsatile arterial bleed might require a combination approach, including mechanical therapy or surgery.
Comparisons with Other GI Bleeding Sites
Mallory-Weiss tears share similarities with other upper GI bleeds, including peptic ulcer disease or Dieulafoy’s lesions. However, the location at or near the gastroesophageal junction can be trickier to manage with mechanical clips in some anatomies.
Lasers, by comparison, can often reach these tears at angles that mechanical devices find challenging.
It’s worth noting that laser therapy is also used for vascular malformations, arteriovenous malformations (AVMs), and even early gastric cancers. Having a versatile laser platform in a GI department can provide solutions for multiple pathologies, not just Mallory-Weiss tear treatment.

Considerations for Clinical Success
Laser therapy is not universally needed for every Mallory-Weiss tear treatment. Many small tears clot and heal on their own, supported by conservative measures such as PPIs and bed rest. Where laser intervention shines is in severe or refractory cases that risk ongoing bleeding if left alone.
Operator expertise is another key factor. Gastroenterologists who are accustomed to injection or clipping techniques may require dedicated training on laser parameters and fiber handling.
By learning to control power settings and angle of approach, they can ensure a rapid, targeted therapy that addresses bleeding without damaging healthy mucosa.
Choosing Laser Wavelength and Power
Different laser wavelengths interact with tissue in distinct ways. For Mallory‑Weiss tears, surface coagulation is the goal, so penetration depth trumps raw wattage.
- 810 – 980 nm diode: Strong hemoglobin absorption, good for shallow vessels, portable consoles.
- 1,940 nm thulium: Higher water affinity, precise for thin mucosa, slightly slower coagulation.
- 10,600 nm CO₂: Peak water absorption, excellent surface sealing, virtually no deep necrosis.
CO₂ remains the benchmark for Mallory‑Weiss tear treatment because its shallow penetration (< 100 µm) minimizes perforation risk at the thin GE junction.

Practical Tips for Implementing Laser Therapy
Medical facilities considering laser-based solutions for Mallory-Weiss tear treatment can improve outcomes by prioritizing thorough staff training and equipment maintenance. Clear guidelines for patient selection and informed consent help ensure the therapy is used appropriately.
Coordinating with the facility’s engineering or biomedical department can streamline the integration of new laser devices.
Partnering with a supplier like International Medical Lasers (IML) provides access not only to advanced lasers but also to educational resources. Quality vendors will offer orientation sessions for clinicians and nurses, covering everything from fiber selection to safe disposal protocols.
Laser Technologies from IML for Mallory-Weiss Tears
IML supplies devices suited to different specialties, including gastroenterology.
While the details of each system may vary, the principle remains the same: precise energy delivery, minimal thermal spread, and robust support for clinicians seeking reliable tools to manage GI bleeding.
Its portfolio covers:
- DEKA platforms — micro‑pulse control ideal for mucosal tears
- Quanta dual‑wavelength systems — CO₂ and diode in one chassis for units managing diverse bleeds
Conclusion
Mallory‑Weiss tear treatments don’t always require advanced tools, but stubborn bleeds can quickly disrupt a day’s surgical schedule.
Laser coagulation offers a fast, gentle way to seal these tears, helping patients recover sooner and freeing up procedure rooms for other cases.
If your endoscopy team is weighing options beyond clips and injections, a CO₂ or dual‑wavelength laser is worth a look.
IML supplies systems that fit standard scopes and provides the training and support you’ll need to put them straight to work.
Curious whether a laser fits your workflow and budget?
Let’s talk through the numbers and clinical data whenever you’re ready.
